The OOP Killer in Yemen’s Crisis Dr. Khalid Shibib
- Introduction
At time of writing this article, the echoes of devastating bombing of Hodeida –Al-Thawra hospital in July and of the school bus in Ṣaʿda in August were ear- deafening and the images across the media horrifying, especially those of dead women and school children. To choose this time to highlight indirect, less visible, yet bigger killer is a challenge that I will try to meet.
The conflict in Yemen, the biggest ongoing humanitarian crisis worldwide, is worsening. The United Nations Yemen Humanitarian Action Plan (YHAP) 2018 identifies 22.2 million persons in need of humanitarian assistance (compared to 15.8 in 2015)[1]
Countries entering into conflict start by having big number of injuries (direct deaths), while continue to have the same list of “peacetime” death causes. As conflict continues, this “peacetime death” occurs at an ever-increasing numbers as indirect result of deterioration of health and socioeconomic condition in the country and decline of health services (indirect deaths). These avoidable excessive indirect deaths take place all over the country, including entirely peaceful regions that are not affected by any war actions. (Figure1 below)
Figure1: Typology of conflict mortality[2]
Experience from 10 conflict-affected countries shows that injuries remain minor killer compared to other causes of conflict- related mortality[3]
In Yemen, Ministry of Public Health and Population (MOPHP) -WHO system reported a total of 65, 717 casualties including 9,604 deaths as of 31 May 2018. Conflict-related Injuries can be used as proxy indicator for severity of conflict, also because of associated infrastructure destruction. Injuries were also associated with severity of first wave of cholera outbreak in 2015-2016[4]. War-related Injuries add to a pre-war cohort of injuries of around 11% (mainly caused by traffic accidents). However, non-communicable diseases (NCD) and childhood diseases (combined with severe malnutrition and infections) and not injuries were the main cause of death before this conflict (see figure 2) and continue to be.
Figure 2: Mortality causes in Yemen[5]
Applying experience from other war-torn countries to Yemen, the main death causes illustrated above would continue throughout the conflict at an ever- increasing rates, possibly changing ranking. The ongoing outbreak of cholera that killed over 2000 persons so far is just an example.
The death at much higher rate of malnourished children, delivering mothers and patients with non-communicable diseases is far “less sensational” and less political than injuries as it lacks the noise of bombardment and shooting and are bloodless.
Saving lives in Yemen : The access drama
Humanitarian access is frequently seen as access of humanitarian actors to target population and priority locations. The YHAP identifies 10 limitations of access humanitarian partners to priority population and areas.
On the other side, Yemeni patients face three major access restrictions to life saving services. These are: unavailability, difficult physical access to and Unaffordability of available life-saving medical services
The unavailability/partial availability of these services is the result of weak coverage of medical services in Yemen, one of the lowest among countries of the region [6]. This limited availability is further reduced by years of decline and shrinkage that has been substantially accelerated during the 3 years of conflict. As an example, according to Health Resource Availability Monitoring System (HeRAMS) in Yemen, out of 3,507 fixed health facilities in Yemen, over 50% have either partially or totally non-functional. Trauma management, maternal and newborn health services as an example were only available in 37% of the facilities. Over 49 districts are without medical doctor.
Physical accessibility is hampered by man-made and natural constraints. YHRP estimates that of the 22.2 million people in need of assistance, approximately 1.5 million people live in districts with the high access constraints[7]. Taking the contraction of health service provision network in Yemen into consideration and the fact that around 70% of Yemen’s population live in rural areas, reaching functional health facilities, especially hospitals, implies travelling for long distance. An additional access barrier is cultural: because of lack of sufficient numbers of female health workers, especially in rural areas, families have to travel longer when having a sick female family member. This is another, additional women-specific mortality factor.
Unaffordability of services is the main message of this paper. Once arriving at the life-saving health facility, patients (and family member) have to pay in cash out of their pocket (OOP) and in advance. Even long before this conflict, around 2/3 of total health expenditure were made out of pocket (cash) by Yemeni citizens and households as shown by successive National Health Accounts (NHA)[8].
Figure 3 (P25 and 34 of NHA 2006) shows contribution of OOP (listed under private) to total health expenditures (left slide) and distribution of these expenditures (right slide).
This Out of Pocket (OOP) spending mainly goes to purchasing medicines; cover hospital expenses, doctor’s fees and costs of surgeries. Lack of operational budget for health facilities and salaries for staff of MOPHP has led to further raising hospital fees (previously moderate fees) to cover part of escalating operational costs. An estimated 30,000 local health workers and operational costs for more than 3,500 health facilities have not been paid for a year [9]. For that, Yemeni patients have to pay more and more official and unofficial fees to get the needed services. De facto, still-functioning public medical care delivery system has been “privatized” and is substantially paid out of pocket. The incomplete funding o UN agencies and NGOs appeals on one side and the crisis of public health sector downloads into skyrocketing demand for the OOP.
The OOP and economic crisis in Yemen [10]
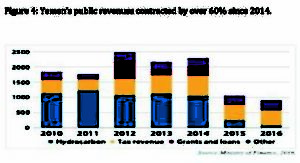
In the past 3 years of conflict, the real GDP in Yemen has been estimated to contract at about 47.1%. This reduction is directly triggered by conflict that has started early 2015 (figure 4)
Figure 4: Yemen’s public revenues contracted by over 60% since 2014.
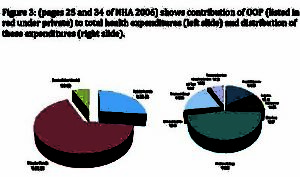
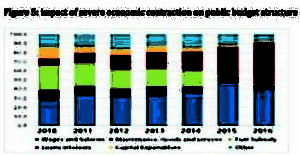
As result, the public sector that provided employment for 31% of the total employees collapsed. State employees, and millions of their dependents haven’t received monthly salaries for more than 14 months. Pensions of more than 41,000 retirees have stopped since March 2017 (Figure 5). Meanwhile, employment opportunities in the private sector have significantly diminished[11].
Figure 5: Within this reduced public budget, its structure also changed. Salaries were irregularly paid mainly to some non-health sectors, operational budget reduced and subsidies to fuel (in green) needed also for hospitals and clinics were removed.
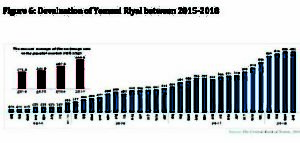
Since 2015-2016, social welfare assistances to 1.5 million cases (households) of the most vulnerable and poorest groups was suspended. The US dollar exchange rate in the parallel market witnessed a significant increase from about YER215 in March 2015 to YER485 in April 2018, an increase of 125.6%. This is turn has substantially increase the prices of all commodities including food but also various medical fees to be paid in cash out of pocket. The devaluation of Yemeni currency destroyed the remaining household capacity to pay out of pocket (OOP).
Figure 6: Devaluation of Yemeni Riyal between 2015-2018
Poverty is a major cause of ill health and a barrier to accessing health care when needed[12]. Poverty as mortality factor has been proved even in advanced economies like the US[13]. In another study, 4.5% of U.S. deaths were found to be attributable to poverty [14]. In Yemen, it is the biggest killer since cash can overcome unavailability of services (through longer travel to those available) and substantial part of their inaccessibility through paying fees out of their pockets whenever inevitable. An increasing part of OOP is the cash to be paid in advance at the facility level, including public, MOPHP –managed facilities, now substantially depending on cash payment by patient at facility level for their survival.
Yemeni patients traditionally look for medical treatment abroad. More than 200,000 Yemenis used to go to Egypt for treatment yearly, with an average expense of $2000 each, summing to $400 million annually, (al Khalil 2010)[15]. It is safe to assume that an equal number of Yemenis goes for treatment in Jordan and other countries. With escalating collapse of health services in Yemen and increase demands as result of deteriorating health conditions, the needs would increase for treatment abroad. However, the restrictions on flying out and back to Sana’a and the deterioration of purchasing power of Yemeni citizens may cause additional mortality on this front. Currently, many Yemeni patients and wounded who managed to came for treatment outside Yemen are stranded in these countries
Conclusion
The main killer in Yemen’s crisis is not war-related injuries but the grave and escalating inability of Yemeni individuals and households to pay out of pocket (OOP) for life-saving interventions against advanced non-communicable diseases, child and maternal diseases. The dramatic deterioration in health care delivery system at a multitude of points (Conflict, contraction of economy, declining public health expenditures) is leading to more and larger out of pocket cash payment by Yemeni citizens who, unlike other system actors, has no escape. However, this citizen has lost most revenues because of economic collapse unemployment, non-payment of salaries for those employed and the dramatic devaluation of Yemeni Riyal. In turn, the ever increasing out of pocket payments is further driving majority of Yemen population into deeper poverty and famine like situation. Only a political solution of Yemen’s conflict can stop and revert the ongoing spiral of economic collapse and related death. This is not about reducing deprivation and suffering. It is about saving lives.
[1] OCHA-Yemen Humanitarian Action Plan 2018 At :
www.who.int/entity/health…/yemen/Yemen-humanitarian-response-plan-2018.pdf
[2] Geneva Declaration 2008 : Global Burden of Armed Violence (P33) At : http://www.genevadeclaration.org/fileadmin/docs/Global-Burden-of-Armed-Violence-full-report.pdf
[3] Guha Sapir et all (2010), quoting the Geneva Declaration 2008 : Demographic and health consequences of civil conflicts, World Development Report, (P15). At : http://web.worldbank.org/archive/website01306/web/pdf/wdr_background_paper_sapir_d%27aoust.pdf
[4]Dureab, F A, et al: Yemen: Cholera outbreak and the ongoing armed conflict. The Journal of Infection in Developing countries, Vol.12 n5, May 2018. At : https://jidc.org/index.php/journal/article/view/10129
[5] WHO (2014): Noncommunicable diseases country profiles-Yemen. At: http://www.who.int/nmh/countries/en/
[6] WHO : World health Statistics 2017 : Monitoring Health for SDGs-Yemen At :
http://www.who.int/gho/countries/yem/en/
[7] OCHA-Reliefweb: Humanitarian access severity Overview July 2018. At : https://reliefweb.int/sites/reliefweb.int/files/resources/Humanitarian_Access_Severity_Overview_July_2018.pdf
[8] MoPHP: National Health Account-Yemen 2006 (P 22). At : http://siteresources.worldbank.org/INTHSD/Resources/376278-1261143298590/6660179-1280173228245/Year2006finalNHAreport.pdf
[9] Health Cluster Bulletin Yemen, September 2017 at : http://www.who.int/health-cluster/countries/yemen/Yemen-Health-Cluster-Bulletin-September2017.pdf
[10] Ministry of Planning and International Cooperation (2018) : Yemen Socioeconomic Update. Issue 34, June 2018 at : https://reliefweb.int/report/yemen/yemen-2018-socio-economic-update-issue-34-june-2018-enar. Slides 4,5 and 6 are taken from this issue.
[11] The World Bank Group (2017) : Yemen Economic outlooks, October 2017 at : https://www.worldbank.org/en/country/yemen/publication/yemen-economic-outlook-october-2017
[12] The World Bank (2014): Poverty and Health at : http://www.worldbank.org/en/topic/health/brief/poverty-health
[13] Peter Dizikes, MIT News office (2016) : New study shows rich, poor have huge mortality gap in U.S. At:http://news.mit.edu/2016/study-rich-poor-huge-mortality-gap-us-0411
[14] Columbia University/ Mailman School of Public Health (July 2011) : How Many U.S. Deaths are Caused by Poverty, Lack of Education, and Other Social Factors. At : https://www.mailman.columbia.edu/public-health-now/news/how-many-us-deaths-are-caused-poverty-lack-education-and-other-social-factors
[15]Al Khalil, Aki (May 2010) : Bad medication exhausts Yemenis funds abroad. Saba News Agency. At: http://sabanews.net/en/print213173.htm
full PDF illustration : The OOPfigures29.08